What is CBT and How Can It Improve Mental Health?
Cognitive Behavioral Therapy (CBT) stands as one of the most extensively researched and widely practiced therapeutic approaches in modern psychology. Developed in the 1960s by psychiatrist Aaron Beck, this structured, time-limited intervention has revolutionized mental health treatment, offering evidence-based strategies for addressing a remarkable range of psychological difficulties. But what exactly is CBT, how does it work, and why has it become such a cornerstone of contemporary mental health care?
The Foundations of Cognitive Behavioral Therapy
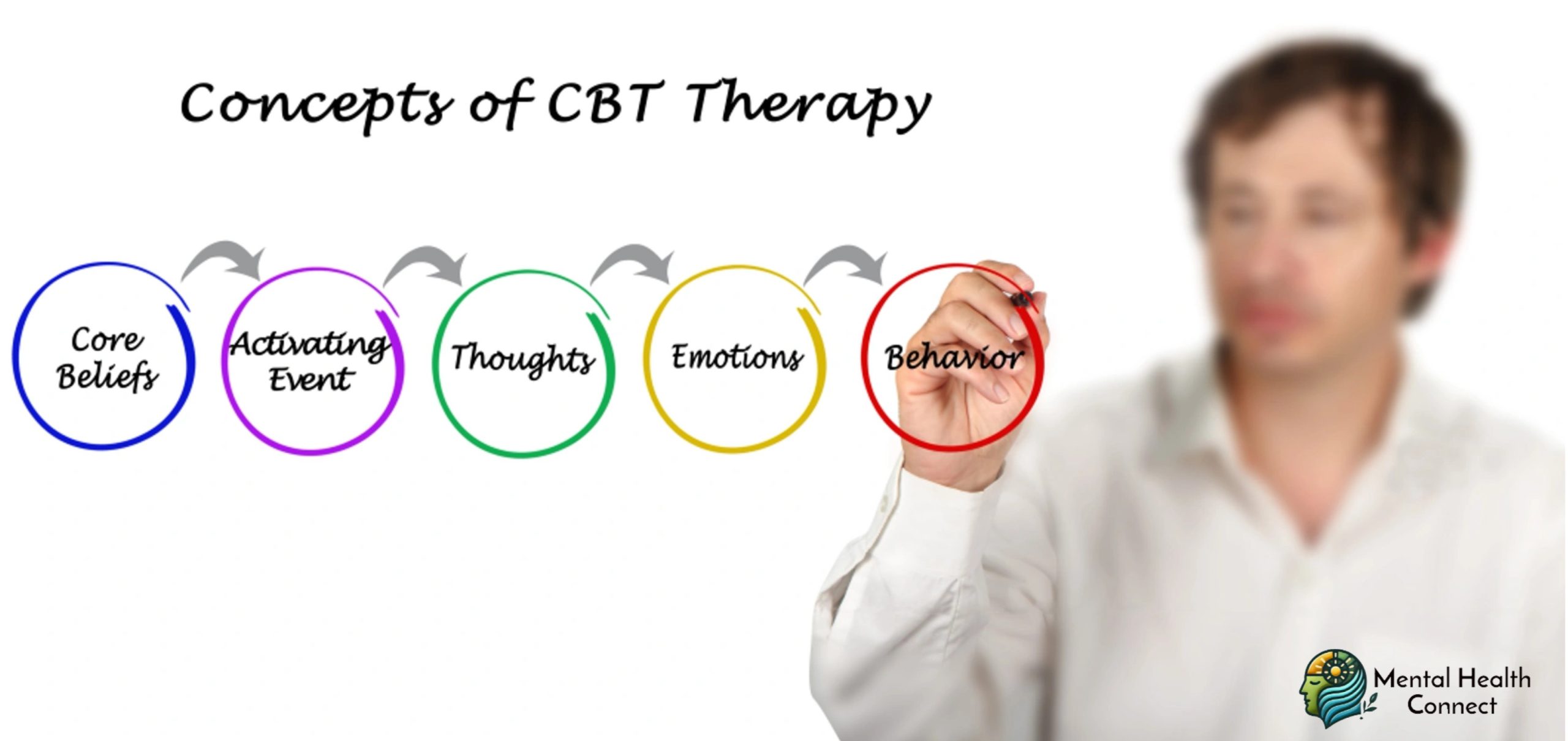
At its core, CBT is built on a straightforward yet profound premise: our thoughts, feelings, and behaviors are interconnected, each influencing the others in powerful ways. This “cognitive model” suggests that it’s not events themselves that determine our emotional responses, but rather our interpretations of those events.
The approach operates on several key principles:
- Cognitive distortions influence emotions and behavior: The way we think about situations often through automatic, unconscious patterns significantly impacts how we feel and act.
- These thinking patterns can be identified and modified: Even longstanding cognitive habits can be recognized and changed through systematic practice.
- Behavioral change can lead to cognitive and emotional shifts: Modifying behaviors, even without directly addressing thoughts, can lead to improvements in mood and thinking patterns.
- Skills-based learning promotes lasting change: CBT emphasizes teaching practical skills that clients can continue using independently after therapy concludes.
Unlike therapies focused primarily on exploring past experiences or unconscious processes, CBT concentrates on current difficulties and practical solutions. It’s active, collaborative, and oriented toward specific goals.
The CBT Process: How Does It Work?
While therapeutic approaches vary somewhat between practitioners, most CBT follows a structured format:
Assessment and Formulation
The therapy begins with a thorough assessment of the client’s difficulties, leading to a shared understanding (formulation) of how thoughts, feelings, and behaviors are maintaining the problem. This typically includes identifying:
- Presenting problems and their history
- Relevant background factors
- Current maintaining cycles
- Strengths and resources
- Goals for therapy
Education and Skill Building
Early sessions often focus on:
- Teaching the cognitive model (the connection between thoughts, feelings, and behaviors)
- Introducing self-monitoring techniques to increase awareness of automatic thoughts
- Developing initial coping strategies for immediate symptom management
Cognitive Restructuring
The core cognitive work involves:
- Identifying automatic negative thoughts and underlying assumptions
- Evaluating the evidence for and against these thoughts
- Developing more balanced, realistic alternative perspectives
- Recognizing and modifying deeper core beliefs when necessary
Behavioral Techniques
Behavioral interventions complement the cognitive work through:
- Behavioral experiments to test the validity of beliefs
- Exposure practices for anxiety-related concerns
- Activity scheduling for depression
- Skills training in areas like problem-solving, communication, or relaxation
Consolidation and Relapse Prevention
Later sessions focus on:
- Practicing skills in increasingly challenging situations
- Identifying potential future triggers
- Developing specific plans for managing setbacks
- Gradually spacing sessions to promote independence
This systematic approach typically unfolds over 8-20 sessions, though treatment length varies based on the complexity of the issues being addressed.
The Evidence Base: What Conditions Does CBT Effectively Treat?
One of CBT’s greatest strengths is its robust research foundation. Hundreds of clinical trials have demonstrated its effectiveness for numerous conditions:
Anxiety Disorders
CBT consistently shows strong efficacy for:
- Generalized anxiety disorder
- Panic disorder
- Social anxiety disorder
- Specific phobias
- Obsessive-compulsive disorder
- Post-traumatic stress disorder
Meta-analyses indicate that 60-80% of individuals with anxiety disorders show significant improvement through CBT, with treatment gains typically maintained years after therapy concludes.
Depressive Disorders
For depression, CBT has demonstrated:
- Comparable effectiveness to antidepressant medication for mild to moderate depression
- Lower relapse rates compared to medication alone
- Particular benefit when combined with medication for severe depression
Other Conditions with Strong Evidence
Research supports CBT’s effectiveness for:
- Insomnia
- Chronic pain management
- Eating disorders
- Substance use disorders
- Bipolar disorder (as an adjunct to medication)
- Anger management
Emerging Applications
Growing evidence supports CBT adaptations for:
- Psychosis
- Autism spectrum disorders
- Attention-deficit/hyperactivity disorder
- Personality disorders
- Grief and complicated bereavement
The versatility of CBT allows it to be tailored to diverse populations across the lifespan, from children to older adults, and adapted for various cultural contexts.
Mechanisms of Change: How Does CBT Improve Mental Health?
Understanding exactly how CBT creates positive change involves several key mechanisms:
Cognitive Shifts
CBT helps individuals develop more flexible, adaptive thinking through:
- Reduced engagement with unhelpful automatic thoughts
- Decreased belief in maladaptive core beliefs
- Development of metacognitive awareness (thinking about thinking)
- Enhanced cognitive flexibility
Behavioral Change
Behavioral improvements often include:
- Reduced avoidance of feared situations
- Increased engagement in rewarding activities
- Improved problem-solving
- Enhanced interpersonal effectiveness
Neurobiological Effects
Research increasingly shows that successful CBT is associated with:
- Normalized activity in the amygdala and prefrontal cortex
- Changes in neural connectivity patterns
- Altered processing of emotional information
- Potential epigenetic modifications
Psychological Resilience
Long-term benefits include:
- Improved emotional regulation skills
- Enhanced self-efficacy and perceived control
- Better stress management capacity
- More adaptive coping strategies
These mechanisms interact synergistically, creating mutually reinforcing cycles of improvement that can continue well beyond the formal therapy period.
Modern Evolutions: How CBT Continues to Develop
While maintaining its core principles, CBT has evolved considerably since its inception:
Integration with Mindfulness
“Third-wave” CBT approaches incorporate mindfulness practices, including:
- Acceptance and Commitment Therapy (ACT), which emphasizes psychological flexibility
- Mindfulness-Based Cognitive Therapy (MBCT), particularly effective for preventing depression relapse
- Dialectical Behavior Therapy (DBT), which balances acceptance and change strategies
Digital Adaptations
Technology has expanded CBT’s reach through:
- Internet-delivered CBT programs with demonstrated effectiveness
- Mobile applications for skill practice and symptom monitoring
- Virtual reality exposure therapies
- Chatbot and AI-assisted interventions
Transdiagnostic Approaches
Rather than disorder-specific protocols, transdiagnostic CBT addresses common underlying processes across conditions, potentially offering more efficient and comprehensive treatment.
Culturally Adapted CBT
Researchers and clinicians have developed culturally responsive CBT versions that:
- Incorporate cultural values and beliefs
- Address culture-specific expressions of distress
- Use culturally relevant metaphors and examples
- Consider collectivist vs. individualist perspectives
These innovations continue to enhance CBT’s effectiveness, accessibility, and applicability across diverse settings and populations.
Practical Applications: Incorporating CBT Principles into Daily Life
While formal CBT is typically delivered by trained mental health professionals, many of its strategies can be adapted for self-help and daily wellness practices:
Thought Records
A simplified thought-challenging process involves:
- Identifying situations that trigger distress
- Noting automatic thoughts in those moments
- Recognizing emotions and their intensity
- Considering alternative perspectives
- Reevaluating the situation
Behavioral Experiments
Testing beliefs through action:
- Identifying a prediction based on a negative belief
- Designing a simple experiment to test it
- Carrying out the experiment and observing results
- Reflecting on what the outcome means for the belief
Graded Exposure
Gradually facing fears:
- Creating a hierarchy of feared situations
- Starting with the least anxiety-provoking item
- Practicing until anxiety decreases
- Progressively moving up the hierarchy
Activity Scheduling
Combating low mood through planned action:
- Scheduling small, manageable activities
- Including a balance of necessary tasks and pleasurable activities
- Rating mastery and pleasure for completed activities
- Gradually increasing activity levels
While these self-help strategies can be beneficial, they work best when aligned with professional guidance for significant mental health concerns.
Limitations and Considerations: When Is CBT Most Appropriate?
Despite its well-documented benefits, CBT isn’t universally effective for everyone or every condition:
When CBT May Be Most Helpful
CBT tends to work particularly well when:
- Specific, identifiable thought patterns are contributing to distress
- The individual is motivated to practice between sessions
- Concrete, measurable goals can be established
- The person has sufficient cognitive capacity to engage with the approach
When Other Approaches May Be Preferred
Alternative treatments might be more appropriate when:
- Trauma processing is the primary need (though trauma-focused CBT is an option)
- Exploring childhood experiences or unconscious processes is central
- Significant personality changes are the goal
- Complex interpersonal issues are the main concern
Complementary Approaches
CBT often works well in conjunction with:
- Medication for certain conditions
- Supportive therapy for processing emotions
- Family therapy for relationship issues
- Motivational approaches for ambivalence about change
The most effective treatment approach should always be determined through collaborative discussion between the individual and healthcare providers, considering unique needs, preferences, and circumstances.
The Promise and Future of CBT
Cognitive Behavioral Therapy has transformed the landscape of mental health treatment, offering evidence-based, time-efficient strategies for addressing a wide range of psychological difficulties. Its emphasis on practical skills, collaborative problem-solving, and lasting change has helped millions worldwide improve their emotional wellbeing and quality of life.
As research continues and the approach evolves, CBT will likely become even more accessible, personalized, and integrated with other effective modalities. Whether delivered through traditional face-to-face therapy, digital platforms, or community-based programs, the principles of CBT provide valuable tools for understanding and improving the intricate connections between our thoughts, feelings, and behaviors.
For anyone struggling with emotional difficulties, exploring CBT either through professional therapy or evidence-based self-help resources offers a pathway toward greater psychological flexibility, resilience, and well-being. The journey may not always be easy, but the potential rewards of more balanced thinking, adaptive behaviors, and improved emotional regulation make it a journey well worth taking.
-
 How to Support Someone with OCDApril 17, 2025
How to Support Someone with OCDApril 17, 2025 -


Leave a Reply